Session 3: Innate Immune Memory
Chairs: Gerd Burmester, Bimba Hoyer
15:20 – 15:45 Steffen Jung
15:45 – 16:10 Chiara Romagnani
16:10 – 16:35 Mihai Netea
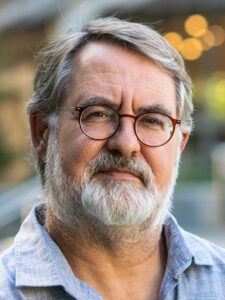
Steffen Jung
Department of Immunology and Regenerative Biology, Weizmann Institute of Science, Rehovot, Israel
Dissecting Monocyte Contributions to Tissue Macrophages in Lung and Brain
Sébastien Trzebanski, Jung-seok Kim and Steffen Jung
Monocytes are short-lived myeloid immune cells that arise from adult hematopoiesis and circulate for a short time in the blood. Monocytes comprise two main subsets, in mice defined as Ly6Clow and Ly6Chigh cells. Classical Ly6Chigh monocytes (CM) are precursors of tissue macrophages. Non-classical Ly6Clow monocytes (NCM) derive form CM and can hence be considered vasculature-resident macrophages.
Recent studies revealed that CM themselves are heterogeneous, including cells with neutrophil- and dendritic cell (DC)-like transcriptomic signatures, that arise from distinct lineages. A fate characterization of these GMP- and MDP-derived CM using adoptive cell transfers and mixed BM chimeras revealed that these cells, surprisingly, differentially seed selected tissues, including the lung and the dura mater during homeostasis and following challenge. Collectively, these data establish a novel link between CM dichotomy to tissue macrophage heterogeneity.
Unlike other tissue macrophages, brain microglia were assumed to original exclusively from macrophages arising in the embryonic yolk sac (YS). However, emerging data from others and us, suggest that the brain microglia compartment of men and mice also harbors monocyte-derived cells. While these cells adopt bona fide microglia signatures and could hence be innocuous, they are, unlike YS-microglia, as HSC progeny targets of clonal hematopoiesis (CH). Indeed, we recently established in a respective mouse model that monocyte-derived microglia that harbor a mutation prominently associated with human CH, DNMT3aR882H, can cause in aging animals nigral neuropathology with Parkinson features.
Biosketch
Born in Homburg/ Saar, Germany, Steffen Jung began his undergraduate studies at the University of Bonn, and then moved to Cologne, where he performed his Ph.D. under the guidance of Andreas Radbruch in the Institute of Genetics headed by Klaus Rajewsky. Specifically, he used the then newly introduced gene targeting technology to define cis-acting control elements driving non-coding ‘sterile’ transcripts in immunoglobulin class switch recombination. In 1993, Steffen moved for post-doctoral
training to Israel and joined the laboratory of Yinon Ben-Neriah at the Lautenberg Center (Hebrew University, Jerusalem) studying transcription factors and kinases in T cell signaling. In 1997, Steffen went to New York for a post-doc with Dan Littman at the Skirball Institute for Molecular Pathogenesis, NYU Medical Center. His studies there focused on the chemokine receptor CX3CR1 and its membrane-tethered ligand CX3CL1. Specifically, he generated CX3CR1gfp reporter mice that have become widely used to study monocyte subsets and brain macrophages. Furthermore, he developed in collaboration with Richard Lang a novel diphtheria toxin receptor (DTR)-based cell ablation strategy and mouse model that allowed the study of dendritic cells (DC) in their in vivo context (CD11c-DTR mice).
In 2002, Steffen returned to Israel and joined the faculty of the Weizmann Institute, where he received tenure in 2009 and full professorship in 2015. Current work of the Jung lab, located in the Department of Immunology and Regenerative Biology, aims at elucidating in vivo aspects of mononuclear phagocytes, including development and differential functions of monocytes and macrophages. Specifically, the team applies intra-vital imaging, conditional cell and gene ablation, combined with advanced genomic analyses to investigate the biology of these cells in physiological health and disease context. Considerable efforts of the Jung lab are dedicated to the development and optimization of research tools. Recent focus is given to the study of blood monocyte subsets, monocyte-derived intestinal and pulmonary macrophages, as well brain macrophages, including microglia and CNS-border associated macrophages.
 Chiara Romagnani
Chiara Romagnani
Charité – Universitätsmedizin Berlin, and German Rheumatism Research Centre Berlin, an Institute of the Leibniz Association, Berlin, Germany
Clonality and long-lasting inheritance of NK cell memory
Clonal expansion of cells with somatically diversified receptors and their long-term maintenance as memory cells is a hallmark of adaptive immunity. With the aim to understand pathogen-specific adaptation within the innate immune system, we study natural killer (NK) cell memory to human cytomegalovirus (HCMV) infection. Leveraging single-cell multiomic maps of ex vivo NK cells and somatic mitochondrial and nuclear DNA mutations as endogenous barcodes, we reveal substantial clonal expansion of adaptive NK cells in HCMV+ individuals. NK cell clonotypes are characterized by a convergent inflammatory memory signature enriched for AP1 motifs superimposed on a private set of clone-specific accessible chromatin regions. NK cell clones are stably maintained in specific epigenetic states over time, revealing that clonal inheritance of chromatin accessibility shapes the epigenetic memory repertoire. Together, our data identify clonal expansion and persistence within the human innate immune system, suggesting that these mechanisms have evolved independent of antigen-receptor diversification.
Biosketch
Chiara Romagnani pursued her medical studies at the University of Florence, Italy, before specializing as an Oncologist at the National Cancer Institute in Genova. Following the completion of her PhD in Immunology at the University of Genova, under the guidance of Lorenzo Moretta, she was granted an EMBO fellowship to train as a postdoctoral researcher at the German Rheumatism Center (DRFZ) in Berlin, Germany. She established there her research focus in innate immunity and inflammation, first as a group leader and later as a DFG-Heisenberg Professor. Her significant contributions include the identification of signals responsible for the differentiation and activation of Innate Lymphoid Cells (ILCs) and the discovery of human innate lymphocyte clonality and memory. Presently, she holds the position of Berlin University Alliance Joint Full Professor at the Charité University and Free University Berlin and serves as the Chair of the Institute of Medical Immunology at Charité – Universitätsmedizin Berlin. Additionally, C. Romagnani holds the role of Chief Editor at the European Journal of Immunology and was recently awarded an ERC Advanced Grant.
 Mihai Netea
Mihai Netea
Radboud University Medical Center, Nijmegen, The Netherlands
Trained immunity: from mechanisms to disease
Induction of trained immunity (innate immune memory) is mediated by activation of immune and metabolic pathways that result in epigenetic rewiring of cellular functional programs. Chromatin accessibility as assessed by histone modifications at the level of promotors (H3K4me3, H3K27Ac) or enhancers (H3K4me1) is an important mechanism mediating these programs. Through network-level integration of transcriptomics, epigenetics and metabolomics data, we identify glycolysis, glutaminolysis, and the cholesterol synthesis pathway as indispensable for the induction of trained immunity by beta-glucan in monocytes. Accumulation of fumarate, due to glutamine replenishment of the TCA cycle, integrates immune and metabolic circuits to induce monocyte epigenetic reprogramming. Furthermore, fumarate itself induces trained immunity, with induction of an epigenomic program similar to β-glucan-induced trained immunity. Identification of the molecular pathways contributing to induction of trained immunity contributes to our understanding of innate immune memory and opens new therapeutic avenues. Finally, the use of inducers of trained immunity to obtain beneficial heterologous effects in infections and cancer will be discussed.
Biosketch
Mihai Netea was born and studied medicine in Cluj-Napoca, Romania. He completed his PhD at the Radboud University Nijmegen, The Netherlands, on studies investigating the cytokine network in sepsis. After working as a post-doc at the University of Colorado, he returned to Nijmegen where he finished his clinical training as an infectious diseases specialist, and where he currently heads the division of Experimental Medicine, Department of Internal Medicine, Nijmegen University Nijmegen Medical Center. He is mainly interested in understanding the memory traits of innate immunity (trained immunity), the factors influencing variability of human immune responses, and the immune dysregulation during bacterial and fungal infections. He is the recipient of the Spinoza Prize 2016 and an ERC Advanced grant in 2019, and since 2016 he is a member of the Netherlands Royal Academy of Sciences (KNAW).
